Urinary Incontinence
Bladder leaks may be common, but they’re never something you just have to live with—our specialists are here to help you find answers and feel in control again.

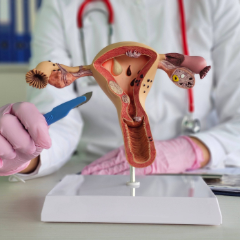
What is Urinary Incontinence in Women?
Urinary incontinence—the involuntary leakage of urine—is more common than you might think, especially among women. Life stages like pregnancy, childbirth, and menopause can weaken the pelvic floor or affect bladder control, leading to leaks with laughter, sneezing, or sudden urges. Whether you’re experiencing stress incontinence, urge incontinence, or a combination of both, the first step to relief is a thorough evaluation. To treat urinary incontinence in women, we use advanced diagnostic tools like urodynamic testing to understand what’s happening and create a personalized plan to help you regain comfort, control, and confidence.
Urinary Incontinence Treatments and Services
We offer a full range of in-office therapies, lifestyle support, and minimally invasive procedures to help you find lasting relief from urinary incontinence.
Pelvic Floor Physical Therapy
Gentle, targeted exercises to help strengthen the pelvic muscles that support bladder control.
Biofeedback Therapy
Using imaging results, we’ll provide real-time guidance on contracting and relaxing your pelvic floor muscles properly.
Urodynamic Testing
This diagnostic testing is done in-office to help evaluate how well your bladder and urethra are functioning.
Lifestyle & Nutrition Counseling
Our urinary incontinence specialist will guide you on bladder-smart habits, fluid intake, weight management, and diet triggers.
Medications
If needed, we’ll provide prescription options to help calm overactive bladder muscles or to support hormone-related changes.
Percutaneous Tibial Nerve Stimulation (PTNS)
This minimally invasive nerve therapy helps improve bladder control with weekly sessions.
Urethral Bulking Injections
A careful, office-based procedure that helps seal the urethra and reduce leaks from stress incontinence.
Minimally Invasive Sling Surgery
This quick-recovery procedure provides long-term support for stress-related bladder leaks.
What’s Causing My Bladder Leaks? Dr. Kahan Explains
In this short video, Dr. Randall Kahan explains what stress urinary incontinence means and why so many women experience it—especially after childbirth or with age. If you’ve ever leaked when you laugh, sneeze, or exercise, this is a must-watch.
We’ll ask you to complete a short intake form and possibly keep a bladder diary for a few days to understand your symptoms better. Our team will also help verify your insurance coverage so there are no surprises.
Your provider will start with a compassionate, judgment-free conversation about your symptoms, lifestyle, and medical history. A physical exam may follow, and if needed, we may recommend simple in-office tests like urodynamic studies to evaluate how your bladder and pelvic floor muscles are functioning.
You’ll leave with a clear understanding of what’s happening and a personalized care plan that fits your needs—whether that’s pelvic floor therapy, lifestyle adjustments, medications, or minimally invasive treatment options. We’ll also be here for follow-up care and any questions you have along the way.
What to Expect During Your Appointment
Insurance Information
Most insurance plans cover the evaluation and treatment of urinary incontinence when medically necessary, though coverage may vary depending on deductibles and copays. Depending on your plan, some procedures or therapies, like nerve stimulation, may require prior authorization. We’ll help you understand your benefits up front, verify coverage, and explore self-pay options if needed—so cost never becomes a barrier to care.
Patient Resources
From accessing the patient portal to downloading forms, reviewing insurance details, and exploring helpful FAQs and educational guides – we make it easy to stay informed, prepared, and confident in your care.
Meet Our Gynecologists


Erin Kopeny, PA-C












Leta M. Vega, DNP, APN, CNM

Gina Marcin, CNM, LAc, RH (AHG)
Alisha M. Wesley, APRN, CNM

Jenny Mathew, WNHP-BC

Claire Bareiss, PA-C

Madison Monk, PA-C, MS
.jpg)
.jpg)

Carter S. Black, RPh







Find a Gynecologist Near You
Choose from five trusted locations across Chicago’s northwest suburbs and get care close to home.
Arlington Heights (Central Rd)
Arlington Heights (Rand Rd)
Buffalo Grove
Kildeer
Schaumburg
Take the First Step Toward Lasting Relief — Schedule Today
Urinary incontinence is the involuntary leakage of urine. It can happen during physical activity (like coughing or sneezing), with a sudden urge to go, or sometimes without warning at all.
It may be common, but it’s not something you have to accept. Bladder leaks are treatable at any age, and many women find relief through therapy, lifestyle changes, or minimally invasive procedures.
Incontinence can result from weakened pelvic floor muscles, childbirth, menopause, certain medications, or conditions like an overactive bladder. Identifying the cause is the first step to finding the right solution.
Stress incontinence causes leaks during movement or pressure (like laughing or lifting), while urge incontinence involves a sudden, intense need to urinate that can lead to accidents. Many women have a mix of both.
We start with a detailed conversation and physical exam, then use tests like a urine analysis or urodynamic studies to understand how your bladder and pelvic muscles function.
We offer a full spectrum of care—from pelvic floor physical therapy and lifestyle coaching to medications, biofeedback, and advanced treatments like Botox injections or sling surgery.
Not necessarily. Many women see significant improvement with noninvasive treatments like biofeedback therapy or nerve stimulation. Surgery is only recommended when other options haven’t worked, and it’s often minimally invasive.
It depends on the treatment, but many patients notice improvement within just a few weeks. We’ll track your progress and adjust your plan along the way.
Most insurance plans cover the evaluation and medically necessary treatments for incontinence. Before we begin, we’ll help verify your benefits and explain any out-of-pocket costs.
It shouldn’t be—and at WomanCare, it isn’t. Our team creates a safe, respectful space where you can talk openly and get the support you deserve.