Menopause Management
Menopause is a natural transition—our role is to help you navigate it with clarity and care that evolves with your needs.

What Menopause Management Means for Your Health
Menopause isn’t just the end of your period—it’s a full-body shift that can affect everything from sleep and mood to bone health and intimacy. Every woman will go through menopause, typically between the ages of 45 and 55, with the average age being about 51, though the symptoms and timing can vary widely. Whether you're navigating hot flashes, memory changes, or vaginal dryness, seeking care isn’t about “fixing” menopause—it’s about managing the transition with confidence, comfort, and personalized support.
Menopause Treatment and Services
For those seeking help for menopause, we offer a range of evidence-based treatments tailored to ease your symptoms and support your long-term wellness.
Hormone Therapy (HT)
This includes low-dose estrogen or combination therapy (estrogen + progesterone) to relieve hot flashes, night sweats, vaginal dryness, and mood changes.
Bioidentical Hormone Therapy (BHRT)
Plant-based hormones—available in pills, patches, creams, or pellets—designed to mimic your body’s natural hormones.
Non-Hormonal Medications
We’ll explore options like SSRIs or gabapentin for hot flashes, as well as treatments for bone health and sleep support.
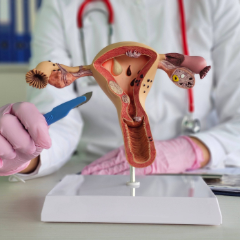
Vaginal Health Therapies
Prescription creams, vaginal estrogen, and laser vaginal rejuvenation to address dryness, irritation, or painful intimacy.
Bone Density Screening (DEXA)
This will identify any early signs of osteoporosis so you can protect your bone strength during and after menopause.
Mood and Sleep Support
If needed, we’ll provide care plans that address irritability, anxiety, insomnia, or cognitive shifts, often in collaboration with mental health providers.
Thyroid and Hormonal Bloodwork
Testing to rule out conditions like thyroid dysfunction or other hormonal imbalances that could affect health.
Your visit begins with a thoughtful conversation. We’ll talk through your symptoms, health history, lifestyle, and how menopause may be affecting your daily life—whether it’s sleep issues, mood shifts, intimacy concerns, or persistent fatigue. This helps us understand your whole picture and tailor your care from the start.
During your exam, your provider will complete a gentle physical exam, which may include a pelvic and breast exam based on your age and symptoms. We may also recommend bloodwork to check hormone levels, thyroid function, and other markers influencing your well-being. If vaginal dryness or discomfort is a concern, we’ll offer options right away.
Afterwards, we’ll review your results and walk through your options—from lifestyle recommendations to hormone therapy or alternative treatments. You’ll leave with a clear care plan, next steps, and a provider who stays with you throughout your menopause journey. Most importantly, you’ll know you have a partner who truly hears you.
Menopause Treatment: What to Expect
Insurance Information
Many menopause-related services—such as annual exams, bloodwork, and evaluations for symptoms like hot flashes or sleep disturbances—are typically covered by insurance when deemed medically necessary. However, coverage for pharmacy prescriptions can vary depending on your insurance plan, deductible, and copay requirements. Our team is happy to help verify your benefits in advance and review self-pay options if needed, so cost never keeps you from getting the care you deserve.
Patient Resources
From accessing the patient portal to downloading forms, reviewing insurance details, and exploring helpful FAQs and educational guides – we make it easy to stay informed, prepared, and confident in your care.
Meet Our Gynecologists


Erin Kopeny, PA-C












Leta M. Vega, DNP, APN, CNM

Gina Marcin, CNM, LAc, RH (AHG)
Alisha M. Wesley, APRN, CNM

Jenny Mathew, WNHP-BC

Claire Bareiss, PA-C

Madison Monk, PA-C, MS
.jpg)
.jpg)

Carter S. Black, RPh







Find a Gynecologist Near You
Choose from five trusted locations across Chicago’s northwest suburbs and get care close to home.
Arlington Heights (Central Rd)
Arlington Heights (Rand Rd)
Buffalo Grove
Kildeer
Schaumburg
Don’t Power Through Menopause Alone
Most women begin menopause between the ages of 45 and 55. Perimenopause—the transitional phase before menopause—can start several years earlier.
Hot flashes, night sweats, sleep problems, mood changes, vaginal dryness, low libido, and memory lapses are all common—and manageable.
If your periods are irregular and you’re experiencing new symptoms like hot flashes or sleep issues, you may be in perimenopause. A blood test can help confirm hormonal shifts.
Yes. Pregnancy is still possible until you’ve gone 12 months without a period. If you’re not planning to conceive, we’ll discuss birth control options.
Not at all. Hormone therapy is just one option. We also offer non-hormonal treatments, lifestyle coaching, and vaginal therapies based on your needs and preferences.
For most healthy women under age 60 or within 10 years of menopause, hormone therapy is considered safe and effective—but we’ll personalize your plan based on your health history.
We offer several treatments, including vaginal estrogen, moisturizers, and laser therapies designed to restore comfort and intimacy.
Hormonal changes can slow metabolism and alter fat distribution. To help manage these changes, we offer nutrition counseling, lifestyle support, and medical guidance.
Yes. Mood swings, anxiety, or depression can emerge or worsen during menopause. It’s important to talk about it—we’ll support you with treatment options that address both body and mind.
We recommend at least one annual visit, or more often if you’re starting a new treatment, managing symptoms, or have ongoing concerns.