Pelvic Pain
Pelvic pain in women is more than discomfort—it’s a signal from your body that deserves answers and relief.

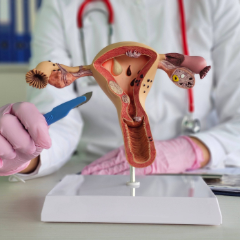
Understanding Pelvic Pain in Women
Pelvic pain in women can feel like a constant ache, a sudden sharpness, or a lingering pressure that’s hard to explain—but always impossible to ignore. For many women, it’s brushed off as “normal” or misunderstood, even when it interferes with daily life, intimacy, or emotional well-being. However, we take your symptoms seriously. Pelvic pain can stem from a wide range of causes, including endometriosis, ovarian cysts, pelvic floor dysfunction, or past surgeries, and our job is to help pinpoint the reason and guide you toward lasting relief. You're not alone in this, and real pelvic pain treatment options are available.
Pelvic Pain Treatment Options
Pelvic Floor Physical Therapy
Gentle exercises and manual techniques to release tension, improve muscle coordination, and reduce pain caused by pelvic floor dysfunction.
Medication Management
Nonsteroidal anti-inflammatory drugs (NSAIDs), hormonal therapies (like birth control or GnRH agonists), or nerve pain medications, depending on the underlying cause.
Minimally Invasive Surgery
Laparoscopy or hysteroscopy to diagnose and sometimes treat conditions like endometriosis, adhesions, or fibroids.
Trigger Point Injections
Targeted pain relief for muscle knots or spasms contributing to chronic pelvic or vulvar pain.
Neuromodulation Therapies
Options like nerve blocks or electrical stimulation (e.g., TENS units) can calm overactive nerves contributing to pelvic or bladder pain.
Hormonal Therapy
When pain is linked to endometriosis, ovarian cysts, or menstrual irregularities, we often recommend hormonal therapy.
Your care starts with a conversation with a pelvic pain specialist. We'll ask about your symptoms, health history, menstrual cycle, past procedures, and any emotional or lifestyle factors that may be contributing to your pain. You don’t need to prepare anything specific, but writing down your symptoms or questions in advance can help you feel more at ease.
Your provider will perform a gentle, focused pelvic exam—only if you're comfortable—and may check for signs of tension, tenderness, or underlying conditions. Depending on your symptoms, we may also recommend imaging (like ultrasound), lab tests, or referrals for pelvic floor therapy. Throughout the visit, you’ll be informed and in control of every step.
We’ll review your findings and create a personalized care plan aligning with your goals. This might include at-home therapies, prescriptions, or follow-up appointments for physical therapy or additional testing. You’ll leave with answers, next steps, and a supportive care team ready to walk the journey with you.
What to Expect During Your Pelvic Pain Visit
Insurance Information
Most insurance plans cover parts of pelvic pain evaluations and related services—such as exams, imaging, lab work—when medically necessary. Coverage for pelvic floor physical therapy may vary and is not always included. For procedures like biofeedback, injections, or minimally invasive surgery, coverage may vary. We’re happy to verify your insurance ahead of time and review any out-of-pocket costs, so you can focus on your care—not the paperwork.
Patient Resources
From accessing the patient portal to downloading forms, reviewing insurance details, and exploring helpful FAQs and educational guides, we make it easy to stay informed, prepared, and confident in your care.
Meet Our Gynecologists


Erin Kopeny, PA-C












Leta M. Vega, DNP, APN, CNM

Gina Marcin, CNM, LAc, RH (AHG)
Alisha M. Wesley, APRN, CNM

Jenny Mathew, WNHP-BC

Claire Bareiss, PA-C

Madison Monk, PA-C, MS
.jpg)
.jpg)

Carter S. Black, RPh







Find a Gynecologist Near You
Choose from five trusted locations across Chicago’s northwest suburbs and get care close to home.
Arlington Heights (Central Rd)
Arlington Heights (Rand Rd)
Buffalo Grove
Kildeer
Schaumburg
Relief from Pelvic Pain is Possible. Let’s Uncover What’s Really Going On.
Pelvic pain can stem from a range of conditions like endometriosis, fibroids, pelvic floor dysfunction, or past surgeries. It can also be due to a combination of physical and hormonal factors.
If your pain worsens during your period, with intercourse, or when using the bathroom—and lasts longer than six months—endometriosis could be a factor.
Yes! Many women find relief through non-surgical options like pelvic floor therapy, hormone management, anti-inflammatory medications, or lifestyle changes. Surgery is only considered when these other treatments aren’t effective first.
Some pelvic discomfort can occur during these transitions, but ongoing or severe pain isn’t something you should “just live with.” If pain interferes with daily life, we recommend getting evaluated.
Pain during sex, called dyspareunia, can be linked to pelvic floor tension, endometriosis, hormonal changes, or scar tissue. It’s treatable—and you deserve care that addresses both physical and emotional impacts.
Pelvic floor dysfunction means the muscles in your pelvic area are too tight, too weak, or not working in sync. Treatments for this often include physical therapy, biofeedback, and guided muscle retraining.
Possibly. Depending on your symptoms, we may use ultrasound, MRI, or minimally invasive procedures like laparoscopy to get clearer answers and personalize your care plan.
Yes. For conditions like endometriosis or ovarian cysts, hormonal contraceptives can reduce inflammation, regulate cycles, and ease pain.
Everybody is different, but many patients notice improvement within weeks of starting treatment.
A gynecologist with experience in pelvic pain and complex gynecologic conditions is a good starting point. At WomanCare, our team includes pelvic pain specialists trained to treat both common and hard-to-diagnose causes.