Hysterectomy
If you believe a hysterectomy may be necessary, you likely have questions or concerns. We’re here to support you through each stage, providing clarity and expert care tailored to your unique situation.

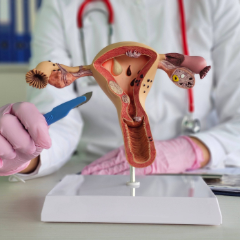
What is a Hysterectomy, and When Is It Recommended
For many women, a hysterectomy—surgery that removes the uterus, and sometimes also the cervix, ovaries, and fallopian tubes—is recommended when other treatments have not alleviated ongoing symptoms. A provider may also recommend a hysterectomy for certain cancers or as a preventive step for those at high genetic risk.
While the decision can feel overwhelming, many patients find relief and improved quality of life after hysterectomy surgery. Recovery typically includes several weeks of rest, with most women gradually returning to normal routines.
- You have heavy or prolonged menstrual bleeding that hasn’t improved with other treatments
- Fibroids are causing pain, bleeding, or pressure symptoms
- You have severe endometriosis that’s not responding to less invasive care
- You’ve been diagnosed with uterine, cervical, or ovarian cancer
- Prolapsed pelvic organs are affecting your quality of life
- Chronic, uterine-related pelvic pain hasn’t improved with other therapies
You’ll have a thorough consultation with your OB/GYN to discuss your symptoms, surgical options, and recovery goals. We'll explain the type of hysterectomy you’ll be having, what organs will be removed, and whether the procedure will be minimally invasive or traditional. You’ll also receive personalized prep instructions to help you feel informed and ready.
Hysterectomy surgery is performed under anesthesia and usually lasts one to two hours, depending on the approach. Our surgical team uses advanced techniques—including minimally invasive options whenever possible—to reduce discomfort and promote faster healing. You’ll be in safe, experienced hands every step of the way.
Recovery looks different for everyone, but most women spend a day or two in the hospital (or go home the same day if having laparoscopic surgery). You may feel tired or sore for a few weeks, so permit yourself to rest. Our team will check in regularly, help manage your symptoms, and guide you in gradually returning to daily activities.
Hysterectomy Surgery: What to Expect
Insurance Information
Most insurance plans typically cover hysterectomy surgery when it is considered medically necessary, such as in cases of fibroids, endometriosis, cancer risk, or abnormal bleeding that has not improved with other treatments. However, coverage for the surgery can vary based on your specific insurance plan, including factors like deductibles and copay requirements. Our team is happy to verify your benefits ahead of time and walk you through any out-of-pocket costs, so you can focus on your care, not the paperwork.
Patient Resources
From accessing the patient portal to downloading forms, reviewing insurance details, and exploring helpful FAQs and educational guides – we make it easy to stay informed, prepared, and confident in your care.
Meet Our Gynecologists


Erin Kopeny, PA-C












Leta M. Vega, DNP, APN, CNM

Gina Marcin, CNM, LAc, RH (AHG)
Alisha M. Wesley, APRN, CNM

Jenny Mathew, WNHP-BC

Claire Bareiss, PA-C

Madison Monk, PA-C, MS
.jpg)
.jpg)

Carter S. Black, RPh







Find a Gynecologist Near You
Choose from five trusted locations across Chicago’s northwest suburbs and get care close to home.
Arlington Heights (Central Rd)
Arlington Heights (Rand Rd)
Buffalo Grove
Kildeer
Schaumburg
Take the Next Step With Support You Can Trust
A hysterectomy is usually recommended to treat chronic issues like fibroids, heavy bleeding, endometriosis, pelvic pain, or certain cancers, especially when other treatments haven’t helped.
That depends on your health needs. Your uterus is always removed, and in some cases, your cervix, ovaries, or fallopian tubes may be removed too. Your provider will explain your specific surgical plan.
Only if your ovaries are removed. If they’re left in place, you may continue to have natural hormone cycles. If your ovaries are removed, menopause will begin right after surgery.
It is a significant procedure, but many hysterectomies today are done using minimally invasive techniques, which means smaller incisions, less pain, and a faster recovery.
Recovery time varies, but most women can return to light activities in 2–4 weeks, with full recovery taking up to 6–8 weeks. We’ll guide your healing every step of the way.
Some patients go home the same day, especially with laparoscopic or robotic procedures. Others may stay 1–2 nights, depending on the type of surgery and how they’re feeling.
If your cervix was removed and you have no history of abnormal cells, you may no longer need Pap smears. Your provider will give you personalized screening guidance.
Yes. Most women can resume sexual activity after about 6 weeks, once healing is complete. Many even report improved comfort if they had pain before surgery.
Only if your ovaries are removed. If they remain, your hormone levels will stay largely the same. If not, we’ll discuss options like hormone therapy to ease the transition.
That’s completely okay. We’re here to answer your questions, explore all options, and help you feel confident in whatever decision you make for your body and your future.